The goal of this project was to cure the patient of her HIV and leukemia diagnoses using stem cell transplants.
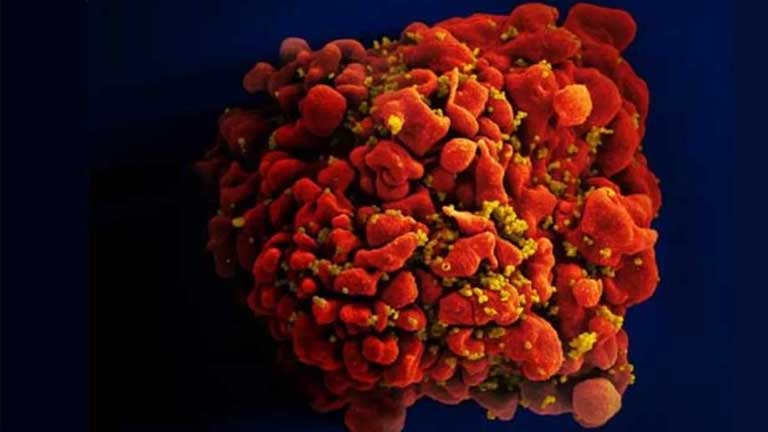
Leukemia clouds the bone marrow with abnormal cancerous cells, preventing the body’s normal blood cells from functioning. HIV attacks the body’s immune system and can be transmitted through bodily fluids and sexual contact with an infected person. Both diseases affect the body’s cells and re-engineer them to attack their host’s body.
Stem cell transplants, originally used to treat cancer diagnoses, are a type of treatment where healthy stem cells are transplanted into a patient’s bone marrow to substitute existing damaged cells.
“Stem cells are going to replace the patient’s immune system and their blood system. The healthy donor cells come in and can recognize any residual cancer cells so they will be able to kill the cells,” said Weill hematologist-oncologist Dr. Jing-Mei Hsu.
A necessary component to the stem cell transplant was finding a Human Leukocyte Antigens identical donor. These antigens are embedded in the immune system and regulate the body’s immune response to foreign materials. Therefore, it is critical that there is a close match between the donor and patient cells to reduce the risks of post-transplant complications.
The HLA type is segregated by ethnicity, with individuals of the African diaspora comprising 10 to 15 percent of donors while Caucasians comprise 70 percent of donors. However, this distinction is important because HLA is needed to match donors to respective patients for blood transplants, Dr. Koen van Basein, director of the Weill/Presbytarian Stem Cell Transplant Program, explained.
van Basein continued that, “Finding a perfectly matching adult donor for this patient was a major step forward since the patient was not Caucasian”.
For the stem cells to properly work, they need to be both HLA compatible and HIV resistant. Because the donor’s cells were not HIV resistant, cord blood cells were introduced, which are stem cells present in the umbilical cord after birth. Cord blood cells are vital to the process because they have mutations in their CCR5 receptors, which is normally an entry point for the virus.
Since cord blood cells are undeveloped and require time to mature into functioning white blood cells, the doctors conducted a second graft of adult stem cells, which were non-resistant to HIV and were a 50 percent HLA match to the patient.
Gradually, the adult graft cells disappeared and the cord blood cells took over as newer HIV resistant cells. van Besien emphasized that the temporary adult stem cells were necessary to protect the patient until the cord blood stem cells grew.
The transplant was a success. Four and a half years later, the patient’s leukemia was cured with no traces of HIV in her system. About fourteen months ago, the patient was officially taken off her HIV antiviral medications and even then, she did not develop any adverse issues nor did her HIV or leukemia resurface.
Dr. Hsu cautioned that the process of transplanting stem cells involves complicated procedures and observations due to the fact that stem cell transplants can be risky as the patient’s body may begin to attack the foreign cells.
“In order for patients to be considered for this treatment, they would need to be selected carefully as it poses a higher risk of infection,” Hsu said.
Nevertheless, this discovery opens pathways for future research in gene and cellular therapy.
Acknowledging that this feat is not indicative of a cure for a majority of HIV patients, Dr. van Besien still notes that Weill has taken a step forward in the research for eventually developing one.
“[T]his process is not a cure for HIV but with some time, it might help us have one for most patients,” van Besien said.