Durham, NC – Results of a phase II clinical trial released today in STEM CELLS Translational Medicine (SCTM) indicate that a limbal stem cell (LSC) transplantation is superior to a tissue graft in treating limbal stem cell deficiency syndrome (LSCD).
This could result in a new and better treatment for LSCD, a condition that is mostly caused by burns to the eye. In its most extreme form, LSCD results in severe vision loss or total blindness. Until recently, the main treatment for this condition was a limbal tissue transplant using tissue from either the patient, a relative or a cadaver — a treatment that carried with it a high risk of rejection and a lifetime of immunosuppressant drugs for the patient.
However, recent advances in cell therapy techniques have introduced stem cell transplantation as a possible way to deal with LSCD. The study reported on in SCTM, conducted by a team of researchers from Centre Hospitalier National d’Ophtalmologie des 15-20 and the Etablissement Français du Sang (EFS), was designed to compare the efficiency and safety of transplantation of LSCs cultured on human amniotic membrane to limbal tissue transplantation.
To do so, the researchers recruited 14 patients with stage 3 LSCD. They treated seven with autologous (their own) limbal stem cells (autoLSC) and seven with allogeneic (donated) stem cells (alloLSC). They followed the patients for an average of 72 months and then compared the results of their treatment to a retrospective control group of 16 people who had received either an autologous or allogenic LSC graft at Centre Hospitalier between 1993 and 2014.
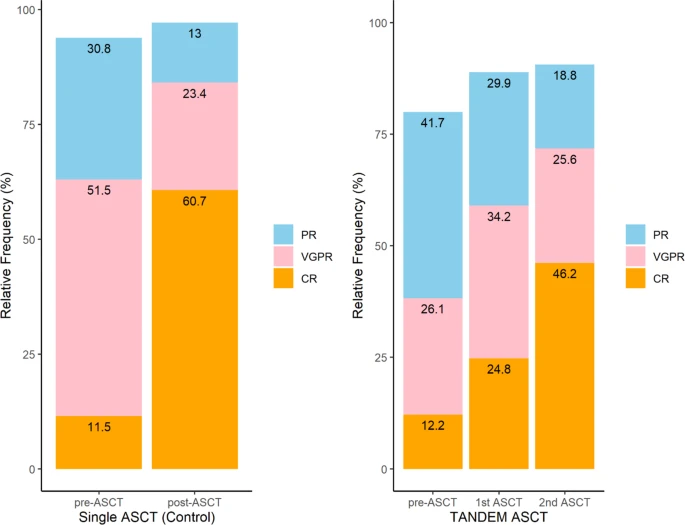
“What we found was that, at the last follow-up visit, visual acuity was significantly better in the autoLSC and autologous limbal tissue (autoLT) groups than in the allogeneic limbal tissue (alloLT) and alloLSC groups. In fact, the allogeneic grafts featured low success rate and serious adverse events,” said Vincent Borderie, M.D., Ph.D., the study’s lead investigator.
“Visual acuity improved by 9.2 lines for autoLSC and 3.3 lines for autoLT,” he added. “And while both the autoLSC and autoLT patients were similar in terms of treatment efficiency — both showed high long-term survival — autoLSC transplantation appears to be safer than autoLT transplantation.”
Specifically, in the autoLSC group, no eyes were found to have decreased vision at last follow up, adverse events were both uncommon and minor, and the size of the limbal biopsy taken in the healthy contralateral donor eye was very small.
“Conversely,” Dr. Borderie said, “in the autoLT group, two out of nine eyes had decreased vision at last follow up, adverse events were common and potentially sight-threatening, and the size of the limbal biopsy taken in the healthy contralateral donor eye was much larger.
“These findings are interesting and useful in considering future cell-based therapies to treat LSC.”
“This study shows that using the patients’ own stem cells to treat a condition that causes severe vision loss or total blindness resulted in vision improvement and was safe to use,” said Anthony Atala, M.D., Editor-in-Chief of STEM CELLS Translational Medicine and director of the Wake Forest Institute for Regenerative Medicine. “These findings are significant, as the cell-based therapy had better outcomes than tissue grafting in the treatment of limbal stem cell deficiency syndrome.”
###
The full article, “Long-Term Results of Cultured Limbal Stem Cell versus Limbal Tissue Transplantation in Stage 3 Limbal Deficiency,” can be accessed at https://stemcellsjournals.onlinelibrary.wiley.com/doi/abs/10.1002/sctm.19-0021.
About STEM CELLS Translational Medicine: STEM CELLS Translational Medicine (SCTM), co-published by AlphaMed Press and Wiley, is a monthly peer-reviewed publication dedicated to significantly advancing the clinical utilization of stem cell molecular and cellular biology. By bridging stem cell research and clinical trials, SCTM will help move applications of these critical investigations closer to accepted best practices. SCTM is the official journal partner of Regenerative Medicine Foundation.
About AlphaMed Press: Established in 1983, AlphaMed Press with offices in Durham, NC, San Francisco, CA, and Belfast, Northern Ireland, publishes two other internationally renowned peer-reviewed journals: STEM CELLS® (www.StemCells.com), celebrating its 37th year, is the world’s first journal devoted to this fast paced field of research. The Oncologist® (www.TheOncologist.com), also a monthly peer-reviewed publication, entering its 24th year, is devoted to community and hospital-based oncologists and physicians entrusted with cancer patient care. All three journals are premier periodicals with globally recognized editorial boards dedicated to advancing knowledge and education in their focused disciplines.
About Wiley: Wiley, a global company, helps people and organizations develop the skills and knowledge they need to succeed. Our online scientific, technical, medical and scholarly journals, combined with our digital learning, assessment and certification solutions, help universities, learned societies, businesses, governments and individuals increase the academic and professional impact of their work. For more than 200 years, we have delivered consistent performance to our stakeholders. The company’s website can be accessed at www.wiley.com.
About Regenerative Medicine Foundation (RMF): The non-profit Regenerative Medicine Foundation fosters strategic collaborations to accelerate the development of regenerative medicine to improve health and deliver cures. RMF pursues its mission by producing its flagship World Stem Cell Summit, honouring leaders through the Stem Cell and Regenerative Medicine Action Awards, and promoting educational initiatives.