Published in Sage Journals – Link to article
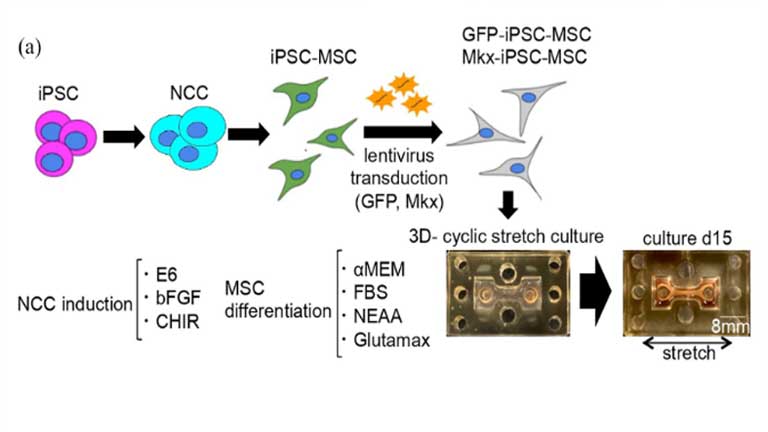
Tendons and ligaments are essential connective tissues that connect the muscle and bone. Their recovery from injuries is known to be poor, highlighting the crucial need for an effective therapy. A few reports have described the development of artificial ligaments with sufficient strength from human cells. In this study, we successfully generated a tendon-like tissue (bio-tendon) using human induced pluripotent stem cells (iPSCs). We first differentiated human iPSCs into mesenchymal stem cells (iPSC-MSCs) and transfected them with Mohawk (Mkx) to obtain Mkx-iPSC-MSCs, which were applied to a newly designed chamber with a mechanical stretch incubation system. The embedded Mkx-iPSC-MSCs created bio-tendons and exhibited an aligned extracellular matrix structure. Transplantation of the bio-tendons into a mouse Achilles tendon rupture model showed host-derived cell infiltration with improved histological score and biomechanical properties. Taken together, the bio-tendon generated in this study has potential clinical applications for tendon/ligament-related injuries and diseases.
Introduction
Tendons connect muscles and bones, and ligaments connect two bones. Both these tissues are critical for transmitting and stabilizing the force produced by muscles and facilitating joint movements.1 Tendon injuries may cause joint motion disability and reduced quality of life.2 There are several treatment options for tendon injuries, including surgical repair or conservative approaches; however, complete cure is difficult and may take time because tendons have low repair capacity, owing to low cell density, and poor innervated blood vessels.3 For instance, Achilles tendon rupture is a frequent tendon injury occurring in 6%–18% of athletes each year and reportedly affects approximately 1 million patients per year in the United States. Once injured, it takes approximately 6 months to return to work.4
Pharmacological approaches and cell transplantation strategies using stem and progenitor cells are under development,5 but their medical application is yet not established.6
Autologous or allogeneic tendons for tendon reconstruction have routinely been applied for medical treatment and have shown relatively good outcomes; however, these materials encounter several problems. Autologous tendon transplantation raises concerns about complications such as pain and nerve damage during graft harvesting.7 When allogenic or xenogeneic tendons are used, decellularization processes are performed to lower their immunogenic effects.8 However, transplantation of xenogeneic tendons may not completely eliminate immunogenicity.9 As for allogeneic tendons, the supply of tissues is limited. Artificial tendons made of polyester and other materials have sufficient tensile strength in the early phase; however, they are not replaced into the recipient tissue; thus, the transplanted material often collapse in the long run.10 In addition, the risk of allergy and infection with artificial materials could also pose problems.11 Dermis-derived tissues have been applied for tendon reconstruction surgery, but their collagen composition and tissue structure differ from those of tendons.12 Moreover, these tissues could not recruit tendon stem/progenitor cells to reconstruct the tendon tissue with proper tendinous matrix formation.13 Based on these facts, an ideal medical strategy to reconstruct tendon ruptures would involve development of an artificial tendon-like tissue with tendon-like mechanical and histological properties from human tendon cells in vitro.
We have previously reported that mouse mesenchymal stem cells overexpressing Mohawk (Mkx) could form a tendon-like tissue in a three-dimensional (3D) cyclic stretch culture system.14 In the present study, we significantly improved the cell stretch chamber system to enable the production of enlarged and well-structured bio-tendons from human induced pluripotent stem cell (iPSC)-mesenchymal stem cells (MSCs) overexpressing Mkx. Aside from the fact that the tissues are derived from human cells, the decellularization process of the bio-tendons should reduce the risk of tumorigenesis and immune reactions associated with the use of allogeneic iPSCs. In fact, we observed significantly improved tendon reconstruction using the newly developed bio-tendon transplant in a mouse tendon rupture model through histological and biomechanical evaluations. Our results support the potential of this bio-tendon for clinical applications.